Each year, Mental Health America publishes the State of Mental Health in America report, which ranks all 50 states and the District of Columbia on 15 mental health access and prevalence measures according to the latest federal data. The conclusion is clear — the U.S. is in a mental health crisis. Americans continue to experience high rates of mental health and substance use conditions and are often unable to obtain care due to cost concerns, lack of coverage, and workforce shortages.
The good news is there are several proposed solutions with bipartisan support. These include addressing youth mental health through social media and early intervention, expanding the workforce (including peer support for young people and adults), and revamping payment incentives that are currently leading to siloed and inadequate care and exacerbating workforce shortages.
The Data
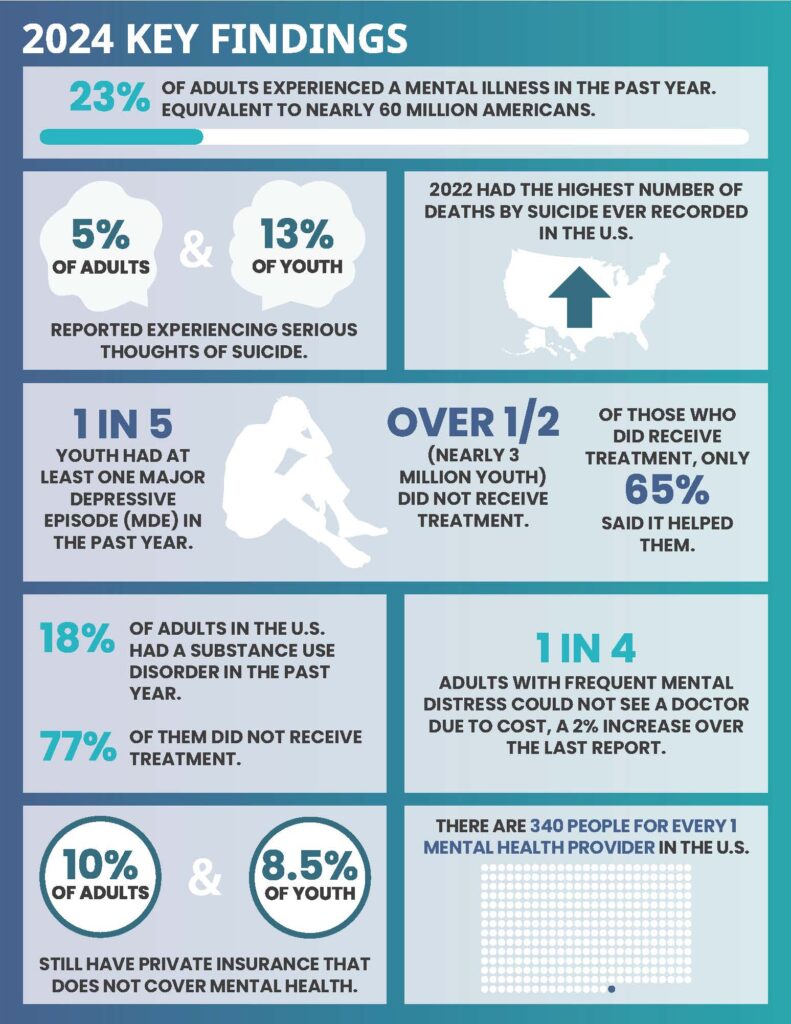
According to the latest data, 23 percent of adults experienced a mental illness in the past year, equivalent to nearly 60 million Americans. After slight decreases in suicide deaths in 2019 and 2020, the number of individuals who died by suicide in 2022 was the highest number ever recorded in the U.S.
According to the latest data, 23 percent of adults experienced a mental illness in the past year, equivalent to nearly 60 million Americans.
The prevalence of behavioral health conditions and suicidal thinking among young people is particularly concerning. More than 10 percent of youth ages 12-17 are experiencing serious thoughts of suicide, nearly one in five is having at least one major depressive episode (MDE), and over half of them — nearly 3 million young people — are not receiving treatment.
Most individuals with substance use disorders are also not receiving treatment. Nearly one in five adults (18 percent) in the U.S. had a substance use disorder in the past year. Of them, 77 percent who needed treatment did not receive it.
Cost and workforce shortages remain significant barriers to accessing mental health care. One in four adults with frequent mental distress could not see a doctor due to cost. In 2022, 10 percent of adults with a mental illness were uninsured and 64 percent of them reported that they did not have health insurance because they could not afford it. Even when people can afford care, they may not be able to access it. There are 320 people for every one mental health provider, and over half of counties lack any psychiatrist.
Recommendations
Prevention and Early Intervention for Youth Mental Health: Making social media safer and more self-directed is critical for promoting youth mental health. According to a Gallup survey, young people are spending on average almost five hours per day on social media platforms. Congress and states should pass legislation to address the addictive nature and mental health harms presented by these platforms. More research and policies should focus on mitigating the harms, while promoting positive social connection and individual choice.
In addition, we need to allocate resources upstream. The Mental Health Block Grant, the largest flexible source of federal funding for local communities, is only available to children who are diagnosed as seriously emotionally disturbed and adults with serious mental illness. In 2022, only 0.67 percent of students were identified as having an emotional disturbance (ED) for an Individualized Education Program (IEP), so very few children are covered. Bipartisan legislation in the House (H.R. 7808) would allow 5 percent of the block grant resources to be used for evidence-based prevention and early intervention activities. This is a start, but more needs to be done to promote an upstream, preventive approach to care and support.

The number of individuals who died by suicide in 2022 was the highest number ever recorded in the U.S.
Workforce Expansion: Growing the workforce for youth peer support is another way to intervene earlier and provide the help and services that young people request. Several bills in Congress would support youth peer programs, including greater research investments, funding for school peer programs, and resources to expand youth peer program workforce development programs at the Health Resources and Services Administration.
For adults, bipartisan, bicameral legislation (H.R. 6748 and S. 3498) would allow health and mental health centers to bill Medicare for peer support services. The addition of peers will improve engagement and coordination with other care providers and ensure that services are tailored to an individual’s goals.
Payment Incentives and Transparency: Finally, federal policy needs to reconsider current fiscal incentives and improve transparency. For example, individuals seeking care often encounter what are referred to as “ghost networks” (provider lists containing numerous inactive listings) and have a very difficult time finding in-network providers. Bipartisan legislation (H.R.7708 and S. 3430) would require greater transparency in Medicare Advantage networks and data on these provider networks should be part of the bonus system to fiscally incentivize and improve access to in-network care.
In addition, Congress should address problematic insurance practices that drive up the cost of care and out-of-network bills, such as step therapy (H.R. 2630 and S. 652) and prior authorization requirements. Rates need to be re-examined, especially for integrated behavioral health care to incentivize primary care practices for adults (H.R. 5819 and S.1378) and children to meet more of the nation’s needs for behavioral health care.
While the current state of mental health in America may be dim, these bipartisan proposals provide reason for hope. With coordinated and persistent commitment, we can intervene earlier, develop the provider workforce, and adequately incentivize an effective system of care.
Schroeder Stribling is the President and CEO of Mental Health America, the nation’s leading community-based nonprofit dedicated to addressing the needs of those living with mental illness and promoting the overall mental health of all. She is a lifelong social justice advocate with over 20 years of experience managing organizations focused on mental health, homelessness, poverty, and racial justice.